Following on from last weeks post about CBCT and childhood cancer. This is a guest post by Alex Ditmarov on when should we be taking a Cone Beam CT of a child.
Alex first published this on his own blog. I thought that it was good and he has allowed us to re-publish this here. I thought that he has put together a really nice summary of an evidence based approach to taking CBCTs on children.
As an aside, I think that his blog is great and it is well worth reading
“When should we take Cone Beam CT of the orthodontic patient?”
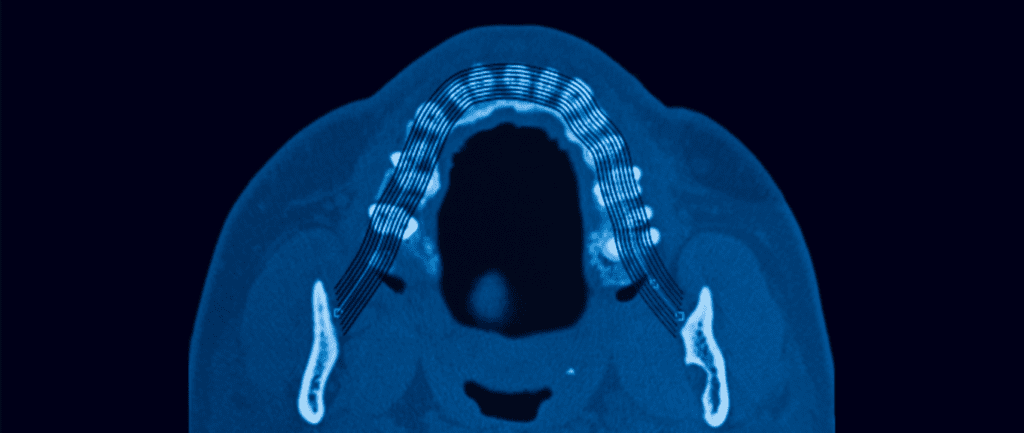
How many times online or during a conference, have we seen a practitioner advocating for the routine use of CBCT? To justify this, the orthodontist often shows the images of scanned airways or primary dentition before and after and say.
“3D images helped me to diagnose airway constriction and crowding. I can’t even imagine how I would now practice without this marvellous technology!”
These, of course, are strong statements and if you look closer, you may find an affiliation of the practitioner with the manufacturer of diagnostic equipment.
So, when should we take a CBCT?
First, I want to look at a study in which 24 orthodontists were asked to evaluate six patients cases with classic diagnostic records and then added CBCT records to the collection of records. They measured the consistency of the examiners treatment decisions with and without the CBCT.
Impact of cone-beam computed tomography on orthodontic diagnosis and treatment planning
Ryan J Hodges et al., Am J Orth, 2013 May;143(5):665-74
DOI: 10.1016/j.ajodo.2012.12.011
They found that the orthodontists did change some of their treatment plans. Importantly, it was in these particular situations:
Importantly, the availability of Cone Beam CT records did not influence the clinical decisions on airway or crowding.
The authors concluded:
“We propose that CBCT scans should be ordered only when there is clear, specific, individual clinical justification.”
Of course, it is a slightly dated and small study. However, more recent and extensive studies only reinforce its findings. For example, I advise you to look at this comprehensive systematic review from 2018:
Annelore De Grauwe et al., EJO, Vol 41, Issue 4, Aug 2019
DOI: 10.1093/ejo/cjy066
The advantages of CBCT over 2D imaging proposed by the authors were:
Here is another relevant study that looks particularly at the airway assessment:
Cone-beam computed tomography airway measurements: Can we trust them?
Daniel Patrick Obelenis Ryan et al., Am J Orth, 2019;156:53-60
DOI: 10.1016/j.ajodo.2018.07.024
Despite the unambiguous message of the AAO white paper on sleep apnea, some practitioners still use CBCT pictures to illustrate the effects of their treatment in enhancing breathing.
The issue with this approach is the fact that the airway is not static. It continually changes during the breathing cycle, and a radiographic image depicts just a particular stage of the process.
The authors included 27 CBCT scans of non-growing patients taken with 4-6 months intervals in their study. One trained operator did all the measurements.
The authors concluded:
“Different CBCT exams with equal scanning and patient positioning protocols can result in different 3D pharyngeal airway space readings.”
In other words, every time you take a CBCT scan, the airway volume measurements would be different.
Indeed, one of the most critical issues of CBCT is its radiation dose. To the day, the effective dose of CBCT scans produced by most machines is many times greater than conventional panoramic examinations.
However, some adepts of routine CBCT examinations state that there is also an option to take low dose CBCT, comparable to panoramic radiographs.
After a PubMed search, I found a paper where the authors indeed claim one particular CBCT machine model is capable of producing extremely low doses.
Phantom dosimetry and image quality of i-CAT FLX cone-beam computed tomography
John B. Ludlow, Cameron Walker, Am J Orth, 2013 May;144(6):802-817
DOI: 10.1016/j.ajodo.2013.07.013
This study’s issue is that the manufacturer paid the authors an “honorarium” – the exact sum is not disclosed. Furthermore, despite the potential positive bias, the authors’ conclusion was still not very persuasive:
“QuickScan+ effective doses are comparable to conventional panoramic examinations. Significant reductions in image quality accompany significant dose reductions. However, this trade-off may be acceptable for certain diagnostic tasks such as interim assessment of treatment results.”
In other words, we probably could limit the dose using a piece of expensive new equipment, however no guarantee we will be happy with the images produced.
Overall, there is no data in the literature to support the indiscriminate use of CBCT in orthodontic diagnosis. We certainly know that CBCT has dramatically expanded our visualisation abilities, but we also have to consider the potential harm of the radiation.
Given the current research data and my clinical experience, here are the situations I take a CBCT scan:
No doubt in the future, we will have new CBCT machines with proven low radiation doses, but until then, we should not put our interests above the patient’s safety.
Link naar het originele artikel: klik hier